As Syphilis Rate Increases, Providers Learn to Identify Oral Symptoms
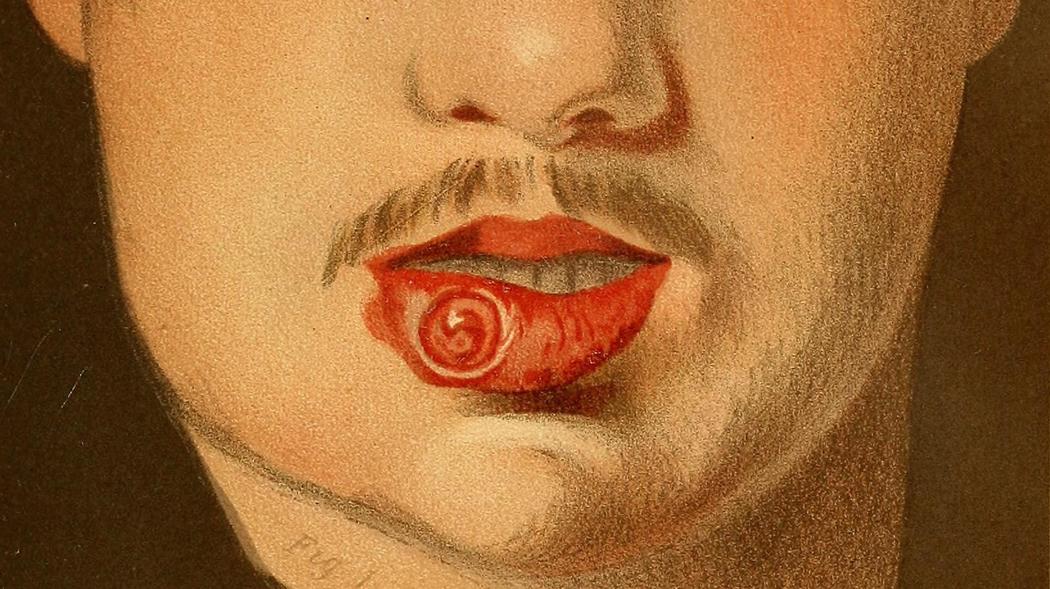 A Victorian medical illustration shows sores on the mouth of a syphilis patient.
A Victorian medical illustration shows sores on the mouth of a syphilis patient.
A spike in syphilis cases, linked to the opioid epidemic, means dentists and other oral healthcare providers should be ready to spot signs of the disease, which often appear in the mouth, said RSM Assistant Professor Dr. Shruti Kashikar.
Although syphilis rates declined after 1943, when penicillin was discovered as a cure, cases began to increase in the early 2000s. Today, rates are at their highest since 1993. Within the past year, there has been an increase of 18 percent of reported cases, totaling nearly 9 cases per 100,000 population, according to the Center for Disease Control (CDC). The disease is transmitted through sexual contact and needle sharing.
“Syphilis is back and it is more important than ever to catch this disease early,'' said Kashikar, who treated two cases of the syphilis during her Oral and Maxillofacial Pathology residency at New Presbyterian Hospital in New York. "Oral manifestations can be seen at all stages of syphilis in men, women and children. It is up to us, as oral health care providers, to diagnose and treat these patients before it’s too late.''
Untreated syphilis can lead to systemic manifestations including heart complications, neurological symptoms, problems with the eyes, bones and skin, and in some cases, death. Before penicillin was used to treat it, patients were often severely disfigured by the disease.
At last month's Research Seminar Speakers series, sponsored by RSDM's Office of Research, Kashikar showed slides of syphilis symptoms that can appear in the mouth, including non-specific ulcers and white mucosal patches on the tongue and lips. Ulcerated lesions that increase in size and firmness, perforations of the palate, and nodular growths on the tongue are other symptoms.
Congenital syphilis, which is transmitted from mother to child during pregnancy, can also present oral symptoms, including "Hutchinson's Teeth,'' which are notched incisors and "mulberry molars,'' which have many small bumps, like the mulberry fruit, said Kashikar. About 40 percent of fetuses and newborns with congenital syphilis don't survive, according to CDC statistics. Children with congenital syphilis can go deaf or blind. Others have severe anemia and bone deformities.
At RSDM, suspected cases of syphilis can be biopsied and those that are confirmed must be reported to the CDC, which tracks syphilis cases. Sexual partners and those who have shared needles with syphilis patients must also be tested for the disease.
Syphilis is most prevalent among gay men and co-infection with HIV can contribute to quicker progression of this disease, although in recent years, the syphilis has spread among intravenous drug users. Rates have also increased among women in the past few years, according to the CDC.
At the start of her lecture, Kashikar delved into the history of syphilis and the misconceptions that have surrounded it over time. In 1494, the first European case was reported in Naples, Italy and many believe that Christopher Columbus’ sailors introduced syphilis in Spain after their voyage from the Americas. It wasn't until later that Europeans realized the disease was sexually transmitted. Early on, they thought it was caused by astrological forces.
Throughout history, attitudes toward syphilis has changed significantly, with blame for the spread of the disease assigned to various people and nationalities. Women, especially prostitutes, were scapegoated for the endemic transmission of syphilis.
"This stigmatization of female sexuality is clearly depicted in art by various artists throughout 18th and 19th century,"said Kashikar. "With time, however, attitudes have changed, along with the demographics of the disease."